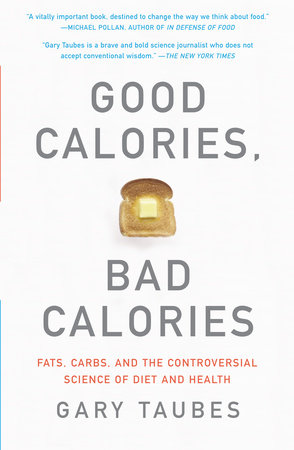
Author Q&A
A conversation withGARY TAUBESauthor ofGOOD CALORIES, BAD CALORIESQ: You make claims in this book that counter everything we’ve been told. You argue that exercise has little or no effect on how much we weigh, that fattening is not about how many calories we eat but what kind of calories we eat. Really?A: I spend the second half of my book making a very simple point: obesity is not a disorder of over-eating or sedentary behavior, but rather a disorder of excess fat accumulation. If you consider obesity as a disorder of fat accumulation, then the natural question is: what regulates fat accumulation? Simple answer: insulin. And what regulates insulin levels? Again a simple answer: carbohydrates. This explains why carbohydrates were considered uniquely fattening from the 1830s until the 1960s. And it explains why carbohydrate-restricted diets, unrestricted in calories (like the Atkins and South Beach diets), seem to be so effective at causing weight loss. One of the most bizarre aspects of the story in Good Calories, Bad Calories is why obesity researchers and clinicians in this country decided that the hormonal regulation of fat tissue is somehow irrelevant to the question of why we grow fat. I still have trouble believing that this actually happened, but it’s all too easy to find obesity authorities who have spent their entire professional careers studying obesity and giving advice, and yet don’t have any idea what hormones actually regulate fat accumulation. Q: Everywhere we look, from Cheerios boxes to New York City’s recent ban on trans fats, we see the message that minimizing dietary fat will help prevent obesity and heart disease. How did we come to believe this “conventional wisdom” and when/how did you begin to doubt it?A: We first came to believe this fifty years ago primarily because a handful of medical researchers of very dubious quality came to believe it unconditionally. They managed to get the American Heart Association to go along, which in turn convinced the health reporters and the politicians and it spread from there. The evidence never came around to support it, but after a while nobody cared. Or at least they didn’t consider the copious evidence refuting the hypothesis to be an impediment to believing that it was true.I came to doubt it initially because I had interviewed some of these people when I was doing an investigative article for the journal Science on the equally unsubstantiated belief that eating salt causes hypertension. My previous two books were about how hard it is to conduct good science, how rigorous and skeptical the scientists have to be, and here I was interviewing these prestigious and respected medical authorities, and they didn’t seem to have a clue what real science was all about. I decided to look into the fat story, knowing nothing about it, simply because these people were involved and claimed to have played significant roles. What I found was the scientific equivalent of a house of cards. These people would do a study to test their beliefs and it would come out either negative or just ambiguous. Then they’d interpret it as supporting their preferred hypothesis—that all fat or just saturated fat was harmful—in light of the fact that there were other studies that also supported their beliefs. And when I looked at the other studies, those were equally ambiguous but were in turn interpreted as supportive because still other studies appeared to support the fat-is-bad hypothesis. And that’s how it went, all the way down and back to the beginning. To mix my metaphors, there was a lot of smoke, but never any fire. Q: Insulin plays a vital role in food digestion. Its function (and dysfunction) is central to Type II diabetes, the most common form of the disease. When we eat certain types of foods (sweets versus fats, refined versus unrefined), what effects do these foods have on insulin levels in the body?A: Insulin is the hormone that our body uses to partition the fuels we consume. It tells us to store fats and protein and burn carbohydrates. So we secrete it when we eat carbohydrates and, to a lesser extent, protein, and the easier it is for us to digest the carbs, the more insulin we secrete. So we secrete more insulin in response to white rice, for instance, than brown rice, or white bread than pumpernickel. Because insulin plays such a fundamental role in how our bodies work, this over-secretion of insulin has profound effects all over. It causes a condition called insulin resistance, which means we have to secrete even more insulin to handle the carbohydrates we eat. The result is this vicious cycle that then seems to lead to virtually every common chronic disease. What it certainly does is make us fat, because insulin works directly on the cells of our fat tissue to tell them to accumulate ever more fat. In general, the higher your insulin levels, the fatter you’ll be.Q: You not only relate the consumption of refined carbohydrates and sugars to weight gain and the escalation of Type II diabetes, you also relate our eating habits to cancer and dementia. Can’t these phenomena be caused by other factors, such as toxic chemicals in our environment?A: It’s possible, but what I’m talking about is a common pattern with all of these diseases. Certainly with cancer, when researchers have looked at the cancer patterns of populations and how their incidence changes over time, they’ve concluded that most cancers are indeed preventable, in that inevitably you can find some population that doesn’t get a particular cancer or gets it at a very low level. But whereas a tiny percent of these cancers might be explicable by pollutants or toxic chemicals in the workplace, the great majority of them seem to be caused by cigarettes and, even more so, by some aspect of our diet or lifestyle. Type II diabetics have a higher risk of Alzheimer’s and cancer, just as they have a higher risk of heart disease and obesity. And when you consider that Type II diabetes is characterized by this condition of insulin resistance, it suggests that having relatively high blood sugar and insulin levels makes you more susceptible to these diseases or even somehow causes them. I looked in the scientific literature for mechanisms that could explain how insulin and blood sugar could actually play a causal role in these diseases, and these mechanisms are very easy to find. So while toxic chemicals in our environment play a role, the evidence suggests that it’s a much, much smaller role than we might think. Diet and lifestyle are more likely culprits, which makes one wonder about foods that raise insulin and blood sugar levels—i.e., refined and easily digestible carbohydrates and sugars. Q: Tell us about the dangers of the high-fructose corn syrup Americans have been consuming in large quantities over the last few decades, just as the rate of obesity has been increasing.A: The dangers of high-fructose corn syrup or HFCS, as it’s called, are real, but we actually pay it too much attention because HFCS in the form that it’s usually found—in sodas and fruit juices and yogurts, etc.—is effectively equivalent to sugar. Both are effectively half glucose and half fructose. It’s the fructose that makes them so sweet. In our bodies, the glucose works to raise our insulin and blood sugar levels. The fructose is dumped directly on the liver, and so increases the amount of fat we store and also, probably, leads to insulin resistance in the long run. When you talk to biochemists who specialize in fructose metabolism, as opposed to say, diabetes specialists who only worry about blood sugar, they’ll tell you that HFCS or table sugar are the worst of all carbohydrates because they have this dual effect.Q: If we want to lose weight (and thus avoid related health problems), can’t we simply eat fewer calories and exercise more? Why focus on carbohydrates versus fats?A: First of all, the actual evidence suggests that eating less and exercising more doesn’t make a bit of difference. Secondly, obese people spend their whole life eating less or at least trying to and it doesn’t help. If it did, they wouldn’t be obese. The fact that a doctor or a health agency or a newspaper reporter tells them they should eat less, doesn’t make it work any better. The thing everyone ignores in this business is that our fat tissue seems to be very well regulated—just as it is in every animal. That’s why we get fat in some places and not in others. We’ve all seen men with big pot bellies and skinny legs. That’s the result of the hormonal regulation of fat tissue. It’s also why men and women fatten differently. Why when men go through puberty they lose fat and women tend to gain it. It’s why women put on fat when they get pregnant. So the obvious question is: what regulates fat accumulation? And it turns out that sex hormones are involved and, more than anything, insulin. Insulin is the only hormone that tells our fat cells to accumulate fat. When insulin levels are elevated, we store fat. And we can’t get rid of that fat without first lowering insulin levels. So what determines how much insulin we secrete? Carbohydrates. It’s actually that simple. As one former Harvard professor of medicine said to me, “carbohydrates is driving insulin is driving fat.” We do not secrete insulin in response to the fat we eat. What else do you need to know? One reason my book is relatively lengthy is because I spend a lot of time explaining why something so simple could be ignored for so long. Q: When you discuss blood cholesterol levels in your book, the evidence you present challenges the emphasis doctors put on lowering cholesterol levels. Should we stop worrying about cholesterol, and if so, why?A: The point is that it’s not the cholesterol itself in the blood that determines your risk of heart disease. It’s not even the LDL cholesterol. It appears to be the LDL particle itself. LDL stands for low density lipoprotein and that’s one of the particles that carries cholesterol and fats around in your blood stream. The idea that cholesterol itself is bad is an idea that dates to the 1970s. Since then, research has shown pretty conclusively that it’s the size and density of the LDL particle that is the risk factor for heart disease. Small, dense LDL is dangerous. Large fluffy LDL is not. And what makes for small, dense LDL: eating a lot of carbohydrates. Fat seems to have no effect. This has been a problem for policy makers, because they’d like to include small, dense LDL as an “official” risk factor for heart disease, but when they try to do so, they’re stuck with this evidence that it’s not fat or even saturated fat that increases the risk of heart disease, but carbs. Q: What do you, as a science journalist rather than a doctor, bring to the subject that will change our minds? A: Perspective. I had no vested interest. I wasn’t taught in graduate or medical school that something was true and so never thought to question it. As a journalist, I question everything. And because my initial training was in physics and I had spent the last 20 years writing about controversial science, I know what’s required to do good science, the need to be skeptical of everything and, perhaps most importantly, to be skeptical of your own pet theories. Once I started my research, I just followed the evidence, not just a study here and there that supports a given point of view but all of the science. All the disciplines, not just a given one. I had no investment in any particular point of view, though I had my hunches based on preliminary research. Some of these hunches turned out to be right; some were wrong. One advantage I had working in the 21st century was that I could do an immense amount of research in a relatively short period of time. The internet allowed me to identify and locate virtually every source, every paper, every book of relevance. Then whatever I couldn’t download or buy or have mailed to me, I had researchers get from various libraries. At one point I had five young researchers working for me, going to different libraries in different cities, getting me the books and articles I needed to make sense of this stuff. Q: What makes us feel hungry? What keeps us feeling full?A: The current theories on hunger all aim to explain what’s happening in the brain that prompts us to eat. Is it leptin levels rising or falling? Glucose? Is it fatty acids? Things like that. The idea I lay out in the book is that hunger and satiety are the body’s response to the ebbing and flowing of fuels at the cellular level. After all, it’s the cells of our tissues and organs that use the fuel. In fact, our brain is pretty much protected against fuel shortages until we’re in the end stages of starvation. So the question becomes: what is it that regulates the availability of fuel at a cellular level? That job once again is handled fundamentally by insulin. One of the things that insulin does is empty the blood stream of available fuel—of glucose and fatty acids. This would explain why true hunger often begins only after we start eating. This is why the first course of a meal is known as an appetizer. It increases our appetite and it does so by prompting us to secrete insulin. The insulin empties our blood stream of fuels, and we get hungry and eat. Because carbohydrates make us over-secrete insulin, they not only make us hungrier than fats and proteins do, but they tend to keep us hungry longer. This is why it’s considerably easier to over-eat carbohydrate-rich foods—pasta, for instance, or popcorn. On the other hand, when we eat foods that are mostly fat and protein, we tend to feel sated.Q: How should the research into nutrition actually be conducted? Why has so little research been conducted effectively?A: The only way to establish with any certainty which foods or diets are healthy in the long run is to do what are known as randomized controlled trials, and to run them for a long time. Take a few thousand or tens of thousands of willing subjects, assign half of them at random to eat one diet and half to another, and keep them at it for a decade or more. This kind of study was planned in the 1960s to test the idea that low-fat diets are good for us, but it never got done because these studies are very hard to do correctly and ludicrously expensive. They can cost hundreds of millions or even a few billion dollars each. The problem is that you can’t know the truth without doing them. So the medical and public health authorities have tried to get around this problem by doing what are called observational studies: look at a huge population people—say, once again, tens of thousands —and try to get an accurate record of what they eat, then follow them to assess their relative health and well-being. But these observational studies can never reliably establish cause and effect. This is a subject I discuss at length in my September 16th New York Times Magazine cover story. These studies can never be trusted to get the right answer, no matter how large they are or how consistently they see the same associations. A lot of the things we’re told these days about what constitutes a healthy diet and lifestyle comes from these observational studies, and there’s simply no way to know if they’re right. As I argue in the epilogue of Good Calories, Bad Calories, we have to bite the bullet and pay for long-term randomized trials—and perhaps figure out more effective ways to do them—or we’ll never know the truth. Q: When you’re not pouring over medical studies, what do you observe about the health and habits of people around you? If you could offer them a few pieces of advice, what would you say?A: It’s hard to spend a significant portion of your life studying diet and health and not want to interject yourself into someone’s life when you see them eating in a way you’ve come to consider unhealthy. Nonetheless, I treasure my friends and family and try to keep my thoughts buried far beneath the surface. If anyone asks for advice, I tell them, of course, to avoid the easily digestible carbohydrates, stay away from sugar in any form, and eat the foods we evolved to eat: meat, fish, fowl, eggs and the non-starchy vegetables.Q: What’s for dinner at your house tonight?A: Well, living in Manhattan and having a kitchen smaller than most peoples’ closets, we tend to have dinner delivered and that decision is always a last minute thing. If it helps any, I had eggs and sausage for breakfast and a hamburger (without the bun) for lunch. I’m a creature of habit.